Metabolic health, especially as it relates to blood sugar regulation, is a fundamental pillar of health. It directly impacts our energy levels, mood, weight, immune function, nervous system, hormones, and even our sleep quality. Based on the Diabetes in Canada report published in 2020, 29% of Canadians live with diabetes or prediabetes and 7.0% live with high blood glucose.1 These are alarming statistics as this comes with increased risk of heart attack, blindness, kidney failure, nerve damage, and amputation.
Are we missing the mark when it comes to preventative screening?
Doctors generally diagnose diabetes by measuring fasting blood glucose and HbA1C, however, normal values for these two parameters does not mean optimal metabolic health. Additional investigations should include the main hormone involved in blood sugar regulation, insulin. ‘Considerations for both tests [HbA1C and fasting insulin] combined identifies highly increased risk for future Type 2 Diabetes in the great majority of white individuals, even those with apparently normal HbA1C’.2 Assessment of insulin, fasting and/or with a glucose challenge, allows for the detection of insulin resistance which precedes the development of type 2 diabetes by 10-15 years.3 Imagine how many people could avoid developing diabetes if they had 10 years to work on it!
What is insulin resistance?
Insulin resistance is a state of impaired biological response to insulin of target tissues, specifically fat, liver, and muscle. At its simplest, this means insulin is less effective at getting glucose out of the blood and into cells. It can present as a wide spectrum of metabolic consequences including:
- Obesity
- Cardiovascular disease
- Metabolic fatty liver disease (previously known as non-alcoholic fatty liver disease)
- Polycystic ovarian syndrome (PCOS)
Type 2 Diabetes can be considered the end state of insulin resistance, the point at which blood sugar levels rise and fall within diagnostic criteria as outlined below4:
- Fasting plasma glucose greater than or equal to 7.0mmol/L or
- HbA1C greater than or equal to 6.5%
- Random plasma glucose greater than or equal to 11.1mmol/L
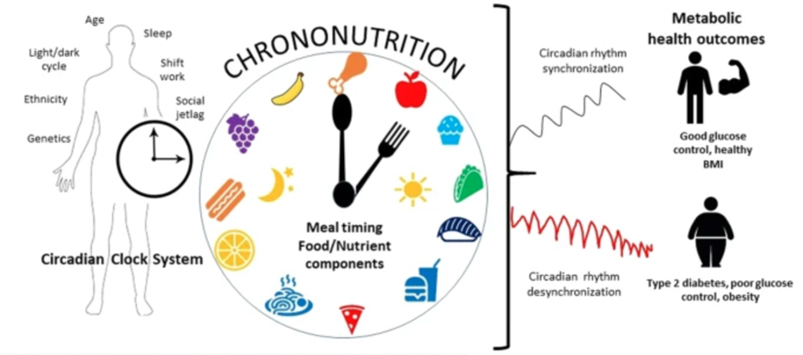
What causes insulin resistance?
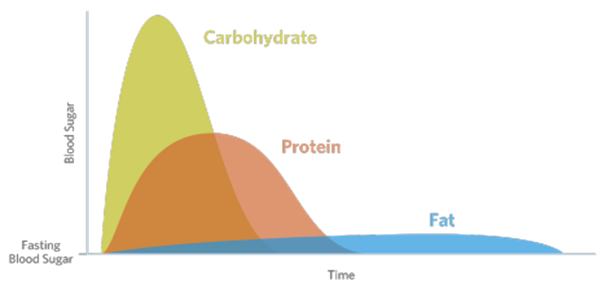
Insulin resistance is multifactorial and often results due to the presence of blood sugar dysregulation, mitochondrial dysfunction, and inflammation. Nutritional and lifestyle practices are main contributors including:
- High simple carbohydrate intake (e.g., bread, rice, sugar, juice)
- Low physical activity
- Weight gain especially around the midsection
- Poor sleep quality (and the presence of obstructive sleep apnea)
Nonetheless, it is important to remember biological processes are never so straightforward and the development of insulin resistance is no different. Additional considerations include:
- Prolonged use medications such as proton pump inhibitors (PPIs) and statin therapy
- Compromised methylation (MTHFR)
- Bile acid metabolism
- Microbiome and dysbiosis (small intestinal bacterial overgrowth)
- Low grade chronic infections
What can you do to support your metabolic health?
Commit and stay consistent with the fundamentals including:
- Eat your fruits and vegetables! They are rich in vitamins, minerals, fibre and most importantly polyphenols which have been shown to increase Akkermansia muciniphila which reduces risk of obesity, inflammation, and insulin resistance.
- Move your body. When it comes to insulin sensitivity, muscle mass is key and general recommendation encourages at least two sessions of strength/resistance training a week for adults.
- Sleep. Matthew Walker, PhD highlights that ‘Inadequate sleep—even moderate reductions for just one week—disrupts blood sugar levels so profoundly that you would be classified as pre-diabetic.’5
For everything else, work with a naturopathic doctor or practitioner that will support you in going beyond what is ‘normal’ and takes a proactive and functional approach to metabolic health.
- Diabetes in Canada: Backgrounder. Ottawa: Diabetes Canada; 2020
- Meigs JB et al. Simultaneous Consideration of HbA1c and Insulin Resistance Improves Risk Assessment in White Individuals at Increased Risk for Future Type 2 Diabetes. Diabetes Care (48), 2020.
- Freeman & Pennings. Insulin Resistance. PMID: 29939616
- Diabetes Canada – Definition, Classification and Diagnosis of Diabetes, Prediabetes and Metabolic Syndrome
- Matthew Walker, PhD. Why We Sleep: Unlocking the Power of Sleep and Dreams. Scribner, 2017.

 647 551 2898
647 551 2898